What is a herniated disc?
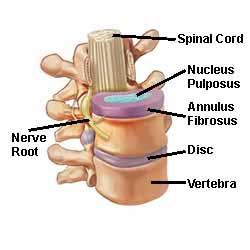
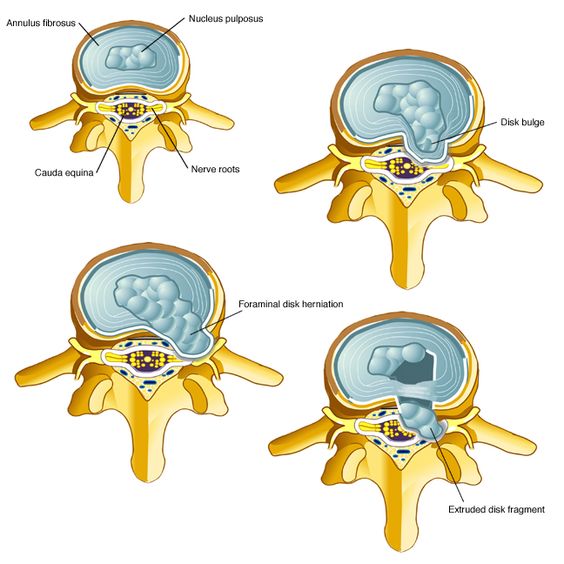
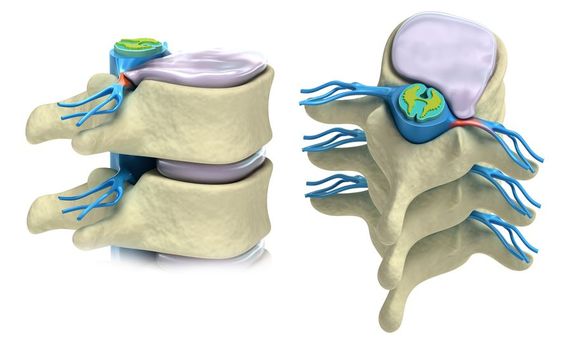
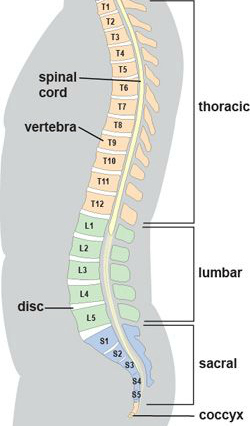
It is helpful to review some spine anatomy before discussing the term herniated disc, also known as a ‘bulging’ or ‘slipped’ disc. In between each bone (vertebra) which makes up the spine, there are discs of soft tissue which act as cushions and allow movement. Known as intervertebral discs, they can be thought of as little jelly doughnuts – jelly on the inside, with a casing on the outside (Fig 1). A herniated disc occurs when there is a tear of the outer casing, which allows the inner gel to bulge out or, in severe cases, extrude into the spinal canal (Fig 2). Not only is a herniated disc painful, the disc material can pinch and/or irritate the exiting nerve root at that level (Fig 3). Although a disc herniation can occur anywhere in the spine, most occur in the lower lumbar spine, between L4, L5, and S1 vertebra (Fig 4).

Fig 1 
Fig 2 
Fig 3 
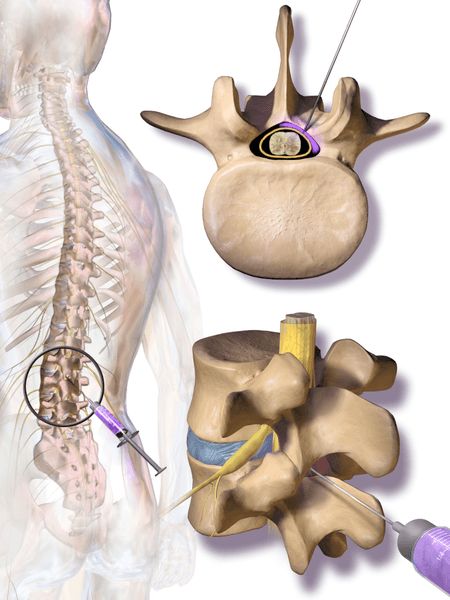
Fig 4
How do we get a herniated disc?
Certain movements, such as twisting in combination with flexion, can squeeze and put sufficient pressure on the intervertebral discs to cause the outer casing to tear. This can be from a single event, however, most cases are due to repetitive strain. Less and less force is required as we get older for this to happen; in fact, many of us in the 4th and 5th decades of life have some degree of disc herniation, but are completely pain free! (MRIs often pick this up as an incidental finding when scanning for some other problem).
What are the symptoms of a herniated disc?
Patients with a herniated disc in the lumbar, or lower spine, typically have leg pain, numbness, or weakness in the area supplied by the affected nerve root, with or without back pain. This condition is sometimes referred to as sciatica. If back pain is present, it typically precedes leg symptoms and is believed to be caused from tearing of the outer casing of the disc itself. Pain is often worse with sitting and relieved with standing. Coughing, sneezing, or straining also makes it worse.
As mentioned, the level of disc herniation determines where in the lower extremities symptoms will be present. Typically, an upper lumbar herniation (L1-2 or L2-L3) results in symptoms above the knee, while a lower lumbar herniation (L3-L4, L4-L5, or L5-S1 causes symptoms that extend below the knee and into the foot. One note of caution here: symptoms involving both legs, particularly involving the inner thighs and buttocks (“saddle anesthesia”), and/or bowel or bladder dysfunctionindicate a rare but much more serious condition known as cauda equina syndrome (CES). Unlike most disc herniations (which involve only one side of the body), CES results from herniation in the central part of the cord. CES requires immediate medical attention, often including surgery.
How is a herniated disc diagnosed?
After a careful history and physical exam, confirmation of a disc herniation is made with an imaging study. Xrays can be helpful, especially if arthritis is present, however, the imaging study of choice is MRI (Fig 5). Highly accurate at imaging soft tissue, the main drawback to MRI (besides cost) is that it can be too sensitive, picking up “abnormal” findings in normal people (see above).

How is a herniated disc treated?
The good news is that the vast majority of those with a disc herniation in the lumbar spine are successfully treated without surgery. The natural history is that, with time, the bulging or extruded part of the disc reabsorbs and decreases in size. Consequently, initial treatment is rest, followed by progressive activity as tolerated. Medications include NSAIDs, muscle relaxants, and occasionally a short course of oral steroids. Physical therapy can be very helpful, particularly back extension exercises.
If symptoms do not respond to rest, therapy or oral medications, an injection corticosteroid is the next treatment step. With both epidural or nerve root injections, long lasting relief can be obtained by applying anti inflammatory medication directly to the site (Fig 6).
Surgery is a last line of treatment for a herniated disc. The indications for surgery are when one has: 1) continued symptoms lasting more than 6 weeks in spite of conservative treatment, including injections, 2) progressive weakness or numbness, or 3) cauda equina syndrome. Many different techniques are used, however, all include removal of at least some of the herniated disc and decompression of the nerve. Recent trends towards minimally invasive techniques (microdiskectomy) have been supported by studies showing shorter hospital stays and less post operative pain compared to traditional methods. Irrespective of the degree of disc pathology or type of surgery chosen, positive predictors for a good surgical outcome include a chief complaint of leg symptoms and/or weakness that correlates with nerve root impingement seen on MRI.
Got a question about this topic? Click here
For more information about this website, click here
References
Orthopaedic Knowledge Update (OKU) 11, Published by the American Board of Orthopaedic Surgeons, 2014, pp 715-725